Malignant melanoma (MM) is the most deadly type of skin cancer. It results from the uncontrolled growth of melanocytes, which are the cells that produce the dark protective pigment in the skin called melanin. About half of all MM evolves from benign or dysplastic moles; the other half appears on previously normal-appearing skin. However, all MM results from the uncontrolled growth of melanocytes. Excessive sun exposure, especially severe blistering sunburns, is believed to be involved in the development of MM. There is also evidence that ultraviolet (UV) radiation used in indoor tanning booths and beds may also be regarded as a possible cause of MM.
MM can appear anywhere on the skin, even in places not directly exposed to sunlight. The most common site is the back for men and the legs for women. Individuals with darker complexions, such as Asians or African Americans, can also develop MM, especially on the palms of the hands, on the soles of the feet, under the nails, and in the mouth.
Most MM will appear on the skin; however, it will rarely appear in an unusual place, such as the inside of the mouth, genital organ, eyes, brain, and respiratory system. If you have risks factors for MM, don’t forget to mention it to your dentist, gynecologist (if you are a female), and ophthalmologist so they can alert you to any unusual growth.
MM is curable when detected early, but if not detected and treated early, it can spread to other organs and become fatal. Once MM has spread inside the body, the cure rate greatly diminishes. The more MM invades the skin, the deeper it becomes and, thus, the more likely it spreads inside the body. MM can spread through the lymphatic channels and/or the bloodstream. If MM does spread, it typically spreads through the lymphatic channel to the lymph nodes draining the area. This is referred to as regional metastasis. The lymph nodes are part of the lymphatic system, a series of vessels throughout the body much like blood vessels that are responsible for collecting and cleaning the body’s fluid in the tissues. These vessels drain to local swellings known as lymph nodes, which are located at various areas on the body. If MM spreads through the bloodstream and reaches other organs, these are called distant metastases. The most common distant metastases of MM are in the skin, lung, liver, brain, bone, digestive system, kidney, and heart.
Risk factors
Anyone can get MM, but there are certain risk factors that make some individuals more susceptible to MM than others. Risk factors increase your susceptibility to MM; however, they do not mean you will develop MM.
Risk factors for MM include
- Personal and family (genetic) history
- Fair skin with red hair and blue eyes
- Male over 50 years old
- Increased number of moles: having more than 50 moles increases the risk of malignant melanoma
- Having atypical or dysplastic moles
- Personal history of AK
- Environmental exposure
- Excessive long-term sun and ultraviolet light exposure
- Fair skin and having grown up in a southern region
- Frequent exposure to outside work or recreation
- History of multiple sunburns
- Freckles
- Use of an indoor tanning lamp or bed
- Medical condition that suppresses the immune system, such as AIDS or medications that organ transplant recipients take to suppress their immune system
- Excessive long-term sun and ultraviolet light exposure
What does MM look like?
There are different types of MM, each type having a different appearance.
- Superficial spreading malignant melanoma is the most common type of MM, accounting for approximately 70% of all MM. This type of melanoma usually starts from a benign or dysplastic mole. Superficial spreading malignant melanoma grows flat on the skin for several months to a few years, penetrating deeper into the skin and spreading inside the body. [Figure 1]
- Nodular melanoma accounts for approximately 20% of all MM. This type of melanoma grows very rapidly and is the most aggressive and deadly type of MM. From the beginning, nodular melanoma grows down into the skin and spreads within a few months inside the body. Usually, this type of melanoma appears as dark black with smooth borders. It is very important to diagnose nodular melanoma as quickly as possible. Any delay in diagnosis can worsen the prognosis and the chances for survival. Nodular melanoma can start from a benign or dysplastic mole and from normal-appearing skin. [Figure 2]
- Lentigo maligna melanoma usually appears on the face and neck as a slowly enlarging brown freckle. Most cases occur in older individuals with excessive long-term sun damage. Lentigo maligna melanoma slowly enlarges, up to the size of a quarter, during many years, becoming asymmetrical and acquiring multiple shades of brown with an irregular border. [Figure 3]
- Acral lentiginous melanoma appears on the palms of hands, on the soles of feet, and under the fingernails and toenails. This melanoma takes several months to a few years to progress. Acral lentiginous melanoma is more common in individuals over 60 years of age with darker complexions. [Figure 4]
- Amelanotic melanoma is a type of nodular melanoma without pigment. It looks like a pink-colored or skin-colored bump without any true features of MM. It is very difficult to diagnose an amelanotic melanoma by inspection of the skin because of the lack of features of MM.

Figure 01

Figure 02

Figure 03
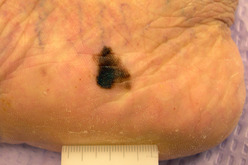
Figure 04
How is MM diagnosed?
Inspection of your skin by your dermatologist can confirm whether or not a mole or growth is suspicious for MM. If your dermatologist determines that a mole is suspicious for MM then a biopsy will be performed. This is a simple procedure performed in the office under local anesthesia. Your mole will then be sent to a pathology lab where thin sections from the mole will be examined under a microscope by a dermatopathologist (a dermatologist or a pathologist trained in the microscopic examination of skin lesions). In the event your biopsy confirms MM, your dermatologist will discuss treatment options.
Inspection of your skin at home with a weekly skin self-exam can help you identify a suspicious mole and help your dermatologist diagnose MM early. [Table 1]
When inspecting your skin for any moles, growths, or spots, look for these signs.
| New | |
|---|---|
| Changing |
|
| Different and/or unusual |
Be suspicious of any new mole or growth, changing mole or growth, or mole or growth that looks different or unusual from those in the surrounding area. If any mole or growth is suspicious, you should immediately report it to your dermatologist as some aggressive types of MM can spread inside your body within a few months.
When inspecting a single mole, only if you know it is a mole, it is helpful to apply the ABCDE rules to determine whether or not it is suspicious. [Table 2]
| Normal | Suspicious | |
|---|---|---|
| Asymmetry |  |
 |
| Border |  |
 |
| Color |  |
 |
| Diameter |  |
 |
| Evolving |
|
|
Asymmetry: malignant melanoma has one half not matching the other half in size, shape, color, or thickness
Border irregularity: malignant melanoma has irregular edges that are notched, ragged, or scalloped
Color: malignant melanoma has a variety of colors within the same lesion, including shades of dark black and dark brown mixed with lighter tones; sometimes it may be red, pink, white, or skin colored
Diameter: malignant melanoma is larger than some surrounding moles, often greater than 6 millimeters or the size of a pencil eraser; however, malignant melanoma is less than 6 millimeters when it first appears
Evolving: malignant melanoma continues to grow and change, while other benign moles remain the same
Treatment options
There are many factors that can influence the choice of treatment:
- Type of MM
- Location, size, number, and aggressiveness of MM
- Patient’s general health
- Side effects, possible complications, benefits, and cure rate of a procedure
- Dermatologist’s experience and familiarity with a particular procedure
Each case is different. Your dermatologist will decide the most appropriate treatment plan for you.
Treatment for MM is dictated by the stage of MM. The stage is determined by the depth of invasion of MM in the skin, which will be measured and reported by a dermatopathologist from the microscopic analysis of the skin biopsy. The patient outcome correlates best with how deep MM has invaded the skin.
Stages of MM
Stage 0 (in situ): MM is found only in the outer layer of the skin, the epidermis, and has not invaded deeper layers. In situ means in the natural or original position.
Stage I: MM is less than 1 millimeter thick with or without ulceration or between 1 and 2 millimeters without ulceration. MM has not spread to nearby lymph nodes. Ulceration means that the epidermis has been destroyed by MM.
Stage II: MM is greater than 1 millimeter thick with ulceration or greater than 2 millimeters thick with or without ulceration. MM has not spread to nearby lymph nodes.
Stage III: MM has spread to one or more nearby lymph nodes or spread to tissues just outside the original tumor.
Stage IV: MM has spread to other organs, to lymph nodes, or to skin areas far away from the original tumor.
If MM is beyond stage I, your doctor needs to learn the extent of the disease before planning your treatment. This is usually done by a team of specialists. The team may include a dermatologist, surgical oncologist, medical oncologist, radiation oncologist, and plastic surgeon. Staging is a careful attempt to learn how deeply MM has invaded the skin, and whether MM has spread to nearby lymph nodes or to other parts of the body. To determine the stage of MM, your doctors may order additional tests, such as a chest x-ray, blood work, and scans of the liver, bones, and brain. To determine if MM has spread to a nearby lymph node, a procedure called a sentinel lymph node biopsy may be performed by a surgical oncologist. The decision on whether to perform a sentinel lymph node biopsy is based on how deep MM has invaded the skin and, in turn, how likely it has spread.
Commonly used procedures to treat MM include:
- Wide local surgical excision
- Sentinel lymph node biopsy and lymphadenectomy
- Chemotherapy and biological therapy
- Radiation therapy
- Picture frame excision of lentigo maligna melanoma
For more information refer to “Common Procedures Performed in Dermatology”.
Treatment choices by stage
Stage 0 (in situ): MM less than 1 millimeter in depth is treated by a wide local surgical excision with a margin of 1 centimeter of normal skin around MM.
Stage I: MM less than 1 millimeter in depth is treated by a wide local surgical excision with a margin of 1 centimeter of normal skin around MM. For MM between 1 and 2 millimeters in depth, a wide local surgical excision with a margin of 2 centimeters of normal skin around MM is performed.
Stage II or Stage III: MM greater than 1 millimeter in depth is treated by a wide local surgical excision with a margin of up to 3 centimeters. Sentinel lymph node biopsy and lymphadenectomy may be performed.
Stage IV: MM greater than 1 millimeter in depth is treated by a wide local surgical excision with a margin of up to 3 centimeters. Sentinel lymph node biopsy and lymphadenectomy may be performed. Radiation therapy, chemotherapy, and biological therapy may also be used.
Prognosis
According to the American Cancer Society, the 5-year survival rate for each stage of MM is as follows:
Stage I: Between 99% and 92%
Stage II: Between 78% and 56%
Stage III: Between 68% and 27%
Stage IV: Approximately 18%
Follow-up care
Patients diagnosed with MM should be examined by their dermatologist at least every 3 months for 2 years, then every 6 months for 3 years, and then once per year for their entire life. Remember, most individuals with a history of MM are more likely to develop another one. Your dermatologist will inspect your skin for any new MMs and will ensure that any previously treated MMs are not growing back.
Patients with a previous history of MM should also perform a weekly skin self-exam. Learning what MM looks like may help you identify a suspicious mole or growth earlier. Inspecting the location of a previously treated MM, as well as the nearby draining lymph nodes, may also help you identify an early recurrence of MM.
If you cannot see some part of your body, ask your partner or a family member to assist you with your weekly skin self-exam.

